Dr. Lindsay Bliss has a passion for patient safety.
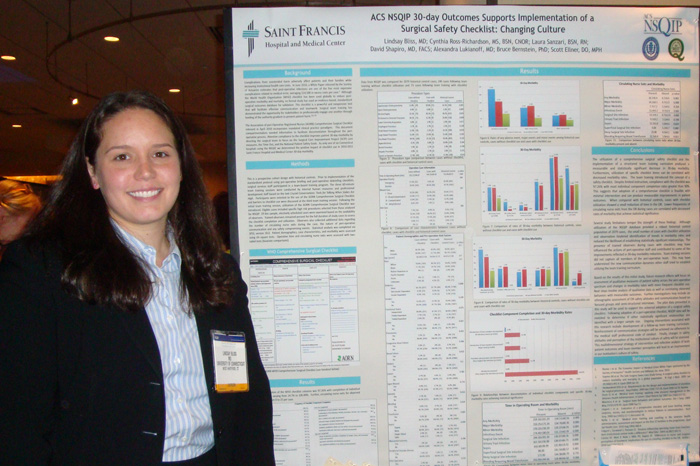
As a fourth-year student at the University of Connecticut School of Medicine, Bliss helped lead an operating room safety project at Saint Francis Hospital and Medical Center studying how using a surgical checklist in the OR could reduce postoperative complications.
She is now in her second year in the UConn Health Center’s general surgery residency, and that passion still burns. Bliss led the study that resulted in the article “Thirty-Day Outcomes Support Implementation of a Surgical Safety Checklist,” published in this month’s Journal of the American College of Surgeons.
“It is an honor to be the lead author of this article,” Bliss says. “The most significant finding of this research is that simple, low-cost interventions such as team communication training and checklist utilization can have a noticeable impact on patient outcomes.”
She and her co-investigators, who included Dr. Alexandra Lukianoff, also a UConn general surgery resident, and Dr. Scott Ellner, an assistant professor of surgery at the UConn School of Medicine and Saint Francis’ director of surgical quality, found that when surgical teams completed both communications training and a surgical procedure checklist before, during, and after high-risk operations, there was a measurable reduction in adverse events such as surgical site infections, blood clots, and urinary tract infections.
“Improving patient safety and outcomes using a cost effective tool was the main motivation for this work,” Bliss says. “Surgeons alter practice patterns based on data and this study provides concrete evidence of the impact team communication training and a safety checklist can have on patient outcomes.”
Bliss and her team used statistics from the American College of Surgeons National Surgical Quality Improvement database of operations done from 2007 to 2010 to establish a baseline group, finding more than 23 percent of those procedures had complications within 30 days.
The results of their study of 319 procedures at Saint Francis between December 2010 and March 2011 showed when surgical teams underwent the communications training only, the 30-day complication rate was 16 percent, and when the communications training was coupled with the surgical checklist, the 30-day complication rate was only 8.2 percent.
“Residents throughout the country are collaborating on significant clinical research and it is wonderful to see that work acknowledged for the scientific merits in publications like JACS,” Bliss says.
“Dr. Lindsay Bliss is an exemplary role model for medical students and residents and an innovative leader in patient safety,” Ellner says.
Bliss says her next research effort will focus on the same interventions and their impact on “the culture of safety in the operating room and the safety attitudes of perioperative staff.
Follow the UConn Health Center on Facebook, Twitter and YouTube.